S2 E9: Learning From Pandemics of the Past
As the world battles the novel coronavirus, University of Virginia history professor Christian McMillen discusses what lessons we can learn — and improve upon — from past pandemics.
How To Listen
Show Notes: Learning From Pandemics of the Past
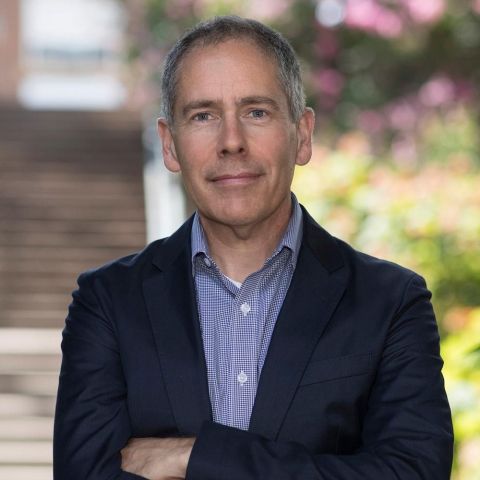
Christian W. McMillen
Christian McMillen researches the history of epidemic disease, as well as American Indian history. He is the author of three books, including “Discovering Tuberculosis: A Global History, 1900 to the Present” (Yale University Press), “Pandemics: A Very Short Introduction” (Oxford University Press) and “Making Indian Law: The Hualapai Land Case and the Birth of Ethnohistory” (Yale University Press).
McMillen’s interest in the history of medicine stemmed from his study of Native American history. His class “Epidemics, Pandemics, and History” is cross-listed with Global Studies, and he has lectured on the topic at the School of Medicine. He is also a member of UVA’s Global Infectious Diseases Institute.
As associate dean for UVA’s College of Arts & Sciences, he manages hiring in all social sciences departments, as well as oversees departmental budgets, tenure and promotion.
Listening to the Show
- Flu of 1918-19
- Competing theories of cholera contraction in the 19th century
- India's 1890s plague epidemic
- World Health Organization
- UVA professors Kevin Cope and Mila Versteeg on Americans' attitudes towards civil liberties during a pandemic
- New York Times | "Covid-19 Changed How the World Does Science, Together"
- “The Great Influenza: The Story of the Deadliest Pandemic in History,” by John M. Barry
- “Faith, Reason and the Plague in Seventeenth-Century Tuscany,” by Carlo M. Cipolla
Transcript
[MUSIC PLAYING]
RISA GOLUBOFF: Hello, and welcome back to Common Law, a podcast from the University of Virginia School of Law. I'm Risa Goluboff, the dean.
LESLIE KENDRICK: And I'm Leslie Kendrick, the vice dean.
RISA GOLUBOFF: A lot has changed in the past few weeks since we recorded our last episode. You've probably noticed we sound a little different. That's because we're calling in via phone now. Like many others figuring out how to work remotely, we're keeping our distance in light of the spread of the novel coronavirus.
LESLIE KENDRICK: Yes. We are in a new world. It's not necessarily one we wanted to be in, but here we are. And because of that, we're going to take a break of sorts with our regular season, which is about when law changed the world, to discuss this new place we're in.
RISA GOLUBOFF: Of course, this pandemic is changing our world in many ways, and we're just starting to realize how many. But pandemics have also had a global impact many times in the past.
LESLIE KENDRICK: The medieval plague, cholera, tuberculosis, the Spanish flu of 1918, HIV-- the list is, unfortunately, long. Today we'll be talking with UVA history professor Christian McMillen about pandemics of the past and what they say about our world today. He's the author of Discovering Tuberculosis: A Global History, 1900 to the Present and Pandemics: A Very Short Introduction. Christian, welcome to Common Law.
CHRISTIAN MCMILLEN: Thank you. I'm happy to be here.
RISA GOLUBOFF: Christian, we're so pleased you could join us. And I'm sorry we couldn't meet together in person. Having written about past pandemics, did you ever think you would see one play out in real time?
CHRISTIAN MCMILLEN: I wish I could say the answer is no, but I've always imagined it-- not because I want to live through the history I write about, but just because I think most historians and other people who think about pandemics-- epidemiologists, public health experts-- I mean, if anything is predictable in world history, it's that another pandemic was coming. And now it's here. So I'm not entirely surprised, though I'm disappointed.
LESLIE KENDRICK: How did you start working on pandemics?
CHRISTIAN MCMILLEN: So before I got into the history of medicine, I was-- I had been working on American Indian history for a long time. And when you're working in American Indian history, it only takes about 5 or 10 minutes to realize how severe infectious disease has been in American Indian history. And I just started getting fascinated by what that looked like long after the early centuries of contact in the 16th, 17th, 18th centuries and how diseases were continuing to affect-- epidemic disease in particular, infectious disease were affecting American Indians into the 20th century, which is really the period I've mostly worked on.
And it turned out that diseases like tuberculosis, particularly others as well, were still-- infectious disease were still the number one killers of American Indians all the way up to the 1960s. And I started seeing connections between the American Indian experience and that of colonized peoples elsewhere. And as it goes in historical research, there's a cascading effect. And it just kept going. So it was really out of my interest and knowledge of American Indian history that I got into history of medicine.
RISA GOLUBOFF: Is there a particular pandemic in the past that reminds you of what's happening today?
CHRISTIAN MCMILLEN: Yeah. You know, I think the one that's probably coming to most people's minds, and mine as well, is the 1918 and then into 1919 influenza pandemic. But there are features of all-- I shouldn't say all pandemics, but many others that come to mind in terms of restrictions on movement or fear or governments handling things ineptly or whatever, cholera in the 19th century in England in particular. So yeah, the 1918 influenza, mostly because-- well, first and foremost, perhaps because of its scope and because of the rapidity with which it traveled the globe.
And unfortunately, because there was a first phase or wave in the spring of 1918-- and we're in the spring of 2020-- where it was severe and traveled fairly wide, but then died down in the summer and then came back in the fall-- and that's where most of the mortality came, was in the fall of 1918. So unfortunately, that's one of the things that comes to mind, knowing that that was the case in 1918. One hopes that won't be the case in 2020.
RISA GOLUBOFF: When you think about the historical comparison, there's the comparison of the pandemic itself, and then there is the comparison of institutions and mobility and communication. And I know a lot of your work is about how institutions have responded in good ways and not good ways. And so when you think about the economic technological institutional moment we're in, do you do you still see the comparisons to 1918? Or how do you think about where we are today compared to the other pandemics?
CHRISTIAN MCMILLEN: I mean, one way in which it's broadly similar is there is no such thing as a coordinated-- I mean, I suppose there's more coordination on the international level now than there than there was in 1918 because we have the World Health Organization, but the responses to influenza in 1918 were really local like they are now. So it's not like Italy, England, France, Germany, Switzerland all did the same thing. They all operated differently, just like we're all doing now.
All 50 states in the United States operated differently. You could have a city like Pittsburgh respond one way and a city like Philadelphia respond another way. I mean, the point being is that there wasn't then, and there isn't really now, a centralized way of responding to pandemics, which I think is-- perhaps that will change after this. I have no idea, of course.
But that's a really broad similarity between the two. The other broad similarity that comes to mind is the sense, in many places, that this is just not a big deal early on, that even though we can see great mortality in Place A, I live in Place B, and it looks like we're going to be just fine. It's just the cold, or it's no worse than the normal annual influenza, which by 1918 was a regular feature of life as well.
So they're not taking it seriously initially. And then the unfortunate other similarity-- and there are more-- but our governments, authorities, public health-- not so much public health people, but, you know, not only not taking it seriously, but restricting the flow of information and not informing the public of really what was going on for-- maybe for some charitable reasons, but also for similar reasons we're seeing now, just wanting to cover up or not admit a lack of preparedness.
LESLIE KENDRICK: Could you give us some examples about different local responses making a big difference back in 1918? I heard anecdotes about decisions to hold World War I victory parades that had dire consequences. What did the patchwork look like?
CHRISTIAN MCMILLEN: Honestly, really similar to now. So you have New York City waiting weeks to start closing public schools or restricting movement or closing movie theaters. You have London doing the same thing, but Manchester acting more quickly. You have Philadelphia taking quite a while to get up and running, but then you have San Francisco having people wear masks, for example. You have some cities closing schools while others didn't. So it's really all over the map. I mean, the examples of local responses are, I would say, as various then as they were now.
I mean, I don't want to be-- to sound so overly critical. And with 20/20 hindsight, we could all go back and tell people what to do. I mean, the speed with which the flu tore through the world in 1918-- where up to somewhere between 50 and 100 million people died in the course of two months, two and 1/2 months-- I mean, no one's prepared for that, and no one could have imagined something on a scale like that. So it's less about-- I mean, it is being critical of some of the real head-in-the-sand approaches, but it's also indicative of just how fast-moving it was that there was not so much time to prepare.
I mean, you read these statements of people who are really cavalier about things, and you think that was wrong. But not knowing exactly what to do is really quite forgivable. And I think that will be the same now, that no one could have imagined this would have-- well, that's not a fair statement. It's hard for many people to imagine something traveling this fast and this widespread and being this serious. None of us have ever lived through it before.
And so it's not surprising that there are local variances in response. What's unfortunate about it is that those local responses seem to range so greatly. I would like to think the band of responses really isn't actually as great as it is.
RISA GOLUBOFF: You mentioned there being commonalities across pandemics, and you mentioned what a couple of those might be. What are the big commonalities that you tend to see in all pandemics?
CHRISTIAN MCMILLEN: Other than mass death, I assume.
RISA GOLUBOFF: Leaving aside the actual pandemic.
CHRISTIAN MCMILLEN: Right.
RISA GOLUBOFF: My question is, what commonalities do we see in responses to pandemics?
CHRISTIAN MCMILLEN: Right, right. Sorry. I couldn't resist.
Yeah, I think the-- god, what are the most-- some of them I mentioned, this notion-- this impulse, it seems, since at least cholera in the 19th century, and perhaps sooner, to either downplay, minimize, or suppress information about the severity of am epidemic or a pandemic. Since the late 19th century and early 20th century, there has been a focus, really, on biomedical approaches to solving the problems of disease, either, A, looking for a vaccine, or B, looking for a cure. And neither of those things are wrong. That would be ridiculous to suggest that we shouldn't look for vaccines or antibiotics.
But you can see now as coronavirus emerges, we have a president who is recklessly suggesting that a vaccine is coming soon and/or a therapy is coming soon-- chloroquine, for example. Meanwhile, we see that there are severe problems with the supply chain. There are severe problems with capacity for dealing with sick people in hospitals. There is no real public health infrastructure to deal with contact tracing.
There is not a coordinated national response. So all of these things that we know could work to mitigate the effects of a pandemic are basic public health measures that, at least in the United States, we've largely let crumble while at the same time assuming and hoping that a magic bullet will come to either, A, give us immunity, or B, cure us. And that's really a function of the century of medical breakthroughs that we would have had in infectious disease.
But tuberculosis has been able to be cured since the 1940s, and really effectively since the late 1950s, yet we now have more tuberculosis than we've ever had in world history despite having a cure. And that's because the conditions that give rise to diseases like tuberculosis are all but ignored while focusing on biomedical interventions. And I think that mindset is common to the response to infectious diseases across the 20th century. And I think it's in evidence today.
I mean, all of these things like social distancing that we're trying to get people to do-- self-isolation, all of this-- these are features of epidemic responses since the 14th century, particularly across early modern Europe. In almost every state in early modern Europe, these were the common ways of dealing with plague particularly, and then reinstituted during cholera in the 19th century, the third plague pandemic in the late 19th and early 20th century.
But now with coronavirus, we've all but forgotten these measures-- I mean, for good reason, in a way. I mean, why would we know about them? But I think it's been a real tradeoff between having a robust public health infrastructure and simply relying on a magic bullet approach to how to deal with epidemic disease.
RISA GOLUBOFF: This is a kind of reverse question of ones you've already answered, but I'm curious if it will yield different kinds of reflections, which are, are there lessons from these earlier pandemics that we could have taken, should have taken, you see us that we are taking, to put it in a more affirmative, positive way? What are those lessons? What do they look like?
CHRISTIAN MCMILLEN: I guess-- I can't take credit for this because I read this in-- John Barry wrote this great book on the flu called The Great Influenza, I think. He may have had two great lessons from the past, but I'm only remembering one, which was for people in power, politicians, et cetera, just to stop lying and tell the truth is probably the greatest thing that we can learn from past pandemics. When people have told the truth, it's had the greatest effect on people's ability to behave in the right way in terms of responding to pandemics, in terms of being able to self-isolate or willfully go into quarantine or whatever.
So it strikes me that-- I agreed with him that's probably the greatest thing we can take from all of these is to stop lying, and that people should listen to experts. I mean, there's an erosion of faith in expertise that's been a part of American culture, anyway, for some time now. And it strikes me that this is probably, at least in my lifetime, the most tragic example of that erosion.
LESLIE KENDRICK: That leads into something that I wanted to ask about. How does the current situation compare with past situations in terms of information transmission, whether that's good information or misinformation? We certainly have a very different information culture and structures than we used to. How does that play out?
CHRISTIAN MCMILLEN: Well, it's a good question. The thing that comes to mind really would be-- is with cholera, for example, in the 19th century. There's extraordinary debate that really had real-world consequences on how diseases were transmitted. Were they transmitted through the air, miasma. You may have heard that phrase before, which just means bad air. Or were diseases contagious and transferred from human to human or by some other vector rather than just the environment or bad air or-- miasma is often referred to rotting vegetable matter producing these gases that come up out of the ground. And that's why you see cholera in some neighborhoods and not others.
And the reason I'm focusing on it is that for a long time after, it was really pretty clear, based on a substantial amount of evidence, that cholera was caused by drinking infected water, infected with cholera vibrio. There was still a tremendous amount, for another 30 to 40 years, of misinformation and medical opinion circulating that, no, no, no, contagion doesn't exist-- it's really miasma-- to the point that one of the last cholera epidemics of the 19th century was in Hamburg, Germany where the public health officials, and thus the public, believed in this theory of miasma and didn't take the same kinds of public health measures that many other cities across Europe had been taking in terms of providing clean water and so forth.
And that strikes me as one of the more apt comparisons of misinformation, people in power simply adhering to the way they've always thought, things they've always believed in the face of overwhelming evidence to the contrary. I think that's what we see now, really, as people calling this just a hoax against Donald Trump or just the flu in the face of overwhelming evidence to the contrary. That strikes me as potentially a historical analogy.
RISA GOLUBOFF: Speaking of how people in power use their power, two of our own professors, Mila Versteeg and Kevin Cope, recently surveyed Americans about their willingness to suspend typical constitutional rights, like the right to gather in houses of worship. And it turned out that the survey respondents were actually quite comfortable with restrictions being placed on those in the name of public health. So in past pandemics, how did people think about such restrictions?
CHRISTIAN MCMILLEN: Yeah, so restrictions on movement and isolation and quarantine have been features of epidemic-- response to epidemic disease, really, since the Black Death in the 1340s, probably most actively rolled out in Italy and then in England in the 16th century, early to mid-16th century-- a whole host of restrictions on movement, public laws prohibiting gatherings like church ceremonies, keeping people in their houses. And then all the way through the end of the 19th century when the bubonic plague came back, particularly the colonial world, really draconian measures of restriction, particularly in places like India, quarantine measures in places like Nigeria during the 1918 influenza pandemic.
And so you have to-- in each instance, there's a level of resistance to all of these measures depending on the time and the place and the context. So for example, one of my favorite little books that I have my classes read whenever I teach my Epidemics class is a book called Faith, Reason, and the Plague in 17th-century Tuscany. And it's a little book that describes-- so Italy, as I said, was one of the very first places that really developed what we would think of as a modern public health system of surveillance and public health hospitals and passing laws to restrict movement and so forth.
And so in the 1630s, when plague came to this little town in Monte Lupo in rural Tuscany, the author of this book, Carlo Cipolla, uses it really quite brilliantly as a way to explore the conflict between faith in the form of the church and then reason in the form of these public health magistrates that are trying to impose public laws against gatherings. And he uses this-- it's this tiny, little micro-history.
The book is very short itself, and it's about this tiny, little place, just a few hundred people, where there's this really intimate battle between this public health official and the bishop of the town who believes that actually, the best way to fight the plague is, in fact, to hold a mass, because the plague is here as a sign of God's wrath. And if we don't have a mass, it will just get worse. And so the public health official says, well, in fact, no, that's perhaps the craziest thing you could possibly imagine doing-- we could possibly imagine doing.
And it results in this really significant conflict that ultimately, there is a fair amount of rioting and resistance, and people flee the town because they don't want to be under quarantine. They don't want to be isolated. So it results in a fair amount of chaos, and it's just an extraordinary story of what the state believes it needs to do, but the citizenry, who is largely Catholic and faithful, thinks it has to do. And then it's a story about the emerging power of the state over that of the church, which has always been the conventional measures or arbiter of power. So that's one example. I mean, there's just a million examples of both resistance to state action and state action itself.
So in India in the 1890s when the plague came back in the Pacific world, and largely affected the colonial world, in particular India-- this is at a time when the British government, especially in the wake of the Laboratory Revolution, is very, very confident in its measures to stamp out infectious disease, but really still doesn't have any idea about how plague itself is transmitted. And so it really approaches it in these draconian ways whereby-- and this is the case in Hong Kong as well. The British government did the same thing there-- burning people's houses down, taking people out of their houses and putting them in isolation, strict quarantine measures that actually backfire to the extent that some public health officials are assassinated. It's one of the major crisis moments in British authority in the colonial world, particularly in Hong Kong and India, the state's response to the plague.
In the colonial world during the flu pandemic, both in Liberia and in Nigeria, significant state-sponsored quarantine measures result in the early-- the beginnings of early anti-colonial movements, because people are so angered and shocked at the draconian measures the state would take to restrict movement and to isolate people and to separate women from men, to bar funeral practices. So yeah, this is a huge feature of the history of epidemic disease.
LESLIE KENDRICK: So that we don't end in such a dark place, are there any hopeful notes you can bring or any guidance you can bring on what we should focus on today to help us all get through this?
CHRISTIAN MCMILLEN: Well, yeah. I mean, I mentioned this-- the way in which people have perhaps over-relied on magic bullets over the last century or so, a little more than that, and have always-- since the Laboratory Revolution and especially since this so-called Golden Age of Medicine in the '50s, '60s, and '70s have over-relied on magic bullets. I mean, there's good reason for that many respects. I mean, it's unfortunate its effects on the diminishment of public health infrastructure, but what's good about it, in fact, is that we actually have a significant-- we've made significant progress on creating vaccines and creating therapies for infectious disease. So it's unfortunate that we're over-reliant, but it doesn't, at the same time, mean that we won't, in fact, develop a therapy or a vaccine.
You know, one of the great stories in the newspaper today was how scientists around the world, more so than perhaps any other time, have been collaborating and not competing with one another, not there's a tremendous amount of competition, necessarily, in this realm of public health. But the level of cooperation and collaboration and goodwill among scientists, no matter where they're from, no matter what country they're from, no matter how high their infection rates are mortality are, they're collectively working to find a vaccine and potentially therapies.
And that's unbelievably encouraging. And I think that earlier, Leslie, you asked about the different forms of communication we have now, how rapidly communication circulates around the world. I mean, this is one of the good effects of the way in which we can be connected is that scientists can work across national boundaries, time zones, et cetera to try and combat something like this. And that collaboration across national boundaries in terms of scientific research has been a feature of global health for decades.
But the speed with which it can happen now and the-- what I gather is the spirit of collaboration is going on now strikes me as unprecedented. And hopefully the results will be rapid and accessible for everyone. I mean, that's one of the great things about it not being a national effort is that by making it an American only effort, it's not-- that means that therapies or the vaccines that will be available will be available accessibly to all rather than nationally based, which would be clearly a tragedy, because if nothing else, I think this should teach us that boundaries and borders and so forth are completely meaningless to microbes.
RISA GOLUBOFF: Thank you so much for this conversation, Christian. It has been so enlightening, and we really thank you for joining us.
[MUSIC PLAYING]
LESLIE KENDRICK: Well, that was really interesting. And Risa, you're a historian, so I assume that you know everything about history. That's just always my starting assumption. But Christian just told us a lot of things that I did not know about the history of pandemics. And it just really is interesting to think about what we're going through right now in that historical context.
RISA GOLUBOFF: I agree. And I appreciate the compliment, but it is utterly not true. And I learned so much from Christian just now. And I will say that one of the things that I found most striking about what he had to say was that the similarities between those past times and this one seemed to come out much more clearly from him than the dissimilarities. And I think we were both, in our own ways, trying to push on where the dissimilarities might be, and transportation, and how quickly things would spread in communication and the nature of the institutions.
And yet it felt like he kept coming back-- he would acknowledge that there was something to that, but he kept coming back to, no, but really, we're doing the same things that we've done before. And we're experiencing similar things. And all of those things that one might think would really make a difference over the last century-- and some of them obviously have. The discussion of vaccines and treatments, that's obviously a totally new world. But then in so many ways, the continuity speaks so much more loudly than the discontinuities.
LESLIE KENDRICK: I think that's exactly right. And I had never thought about social distancing being a very old idea and that there are practices that people have engaged in for a long time to ward off disease when they didn't have all of the modern medical tools that we have that are still, in many ways, our first line of defense.
And of course, we're using them now just as people have used them in the past. They're unfamiliar to us, and we haven't ever-- thank goodness-- had prior need to use them in our lifetimes. But they are tried and true, and they're an important part of our arsenal right now.
RISA GOLUBOFF: Yeah. And it's striking also the differences in how we're using them and how-- the stories about how different localities responded differently in the past. And you might think, especially given national governments, international institutions, the rise of public health in the 20th century, that the local response wouldn't matter as much today, and yet we're seeing that it really does and that it still seems to be making the kind of difference that it made in 1918 when some cities had their parades and others didn't. And we're still seeing that play out very publicly and very visibly in the way the pandemic is spreading.
LESLIE KENDRICK: And in some ways, I think that's one of the most hopeful, and also one of the most worrying, things about it. Because on the hope side, individual decisions that we all make can make a big difference, and decisions that individual localities make can make a big difference. I think on the more worrisome side, as Christian noted, microbes don't respect boundaries. And so coordination could be a really important tool in trying to fight this problem.
But we can feel like we're making a difference in our own backyard. Maybe literally by staying in our own backyard, we can make a difference.
RISA GOLUBOFF: Yes, I think that's right. And I think also, it's not only about our locales or our governments. It's also about our institutions. And from where we sit in a law school and a university, we've really watched universities and colleges and educators around the world responding in similar ways to try to disperse their people and continue their missions, but doing so remotely to try to protect not only the folks within our own communities, but the larger public health. And we've all been working on this within our own context. And it's-- I think it's so important to lift our heads up and listen to Christian and think about the larger global and historical context in which this is all happening.
LESLIE KENDRICK: I completely agree. And we're doing it. The law school is doing it. The university is doing it along with universities across the country and schools across the world and different types of businesses and enterprises and institutions across the world. And we're all focused on how to make it work-- in our case, how to continue education at a distance through online learning. And there are lots of operations questions that go along with that.
But the operations here-- really, they are operational questions, and we can get our hands around them. And we're doing that in the interest of forestalling much larger public health issues that we're all looking at. And we're trying our best to mitigate them. And it's nice to be reminded that we're doing this all together and that it's exactly what people have done in the past.
[MUSIC PLAYING]
RISA GOLUBOFF: That's it for this episode of Common Law. Join us next time when we'll return remotely for more stories about when law changed the world.
LESLIE KENDRICK: Until then, we hope you and your loved ones stay healthy and safe. If you have time, tell us what you think. Rate or review us on Apple Podcasts or wherever you hear the show. To learn more about this episode and others, visit us at commonlawpodcast.com or follow us on Twitter @CommonLawUVA.
RISA GOLUBOFF: In two weeks, we'll be back with our next guest, UVA Law Professor Saikirshna Prakash. He'll be discussing his new book, The Living Presidency, about the rise of presidential power.
LESLIE KENDRICK: Common Law comes to you from the University of Virginia School of Law. Today's episode was produced by Sidney Halleman, Robert Armengol, and Mary Wood with help from Virginia Caine. This show is being recorded on our iPhones. I'm Leslie Kendrick.
RISA GOLUBOFF: And I'm Risa Goluboff. Be well, and we'll see you next time.
[MUSIC PLAYING]
